Urogynecology
(Female Pelvic Medicine and Reconstructive Surgery) - is a sub-specialty of obstetrics and gynecology dedicated to the treatment of pelvic floor disorders, such as problems with tissue relaxation (prolapse), urinary, bowel, and sexual dysfunction. These diseases include the inability to control your bladder, pelvic organ prolapse, urinary incontinence, fecal incontinence, constipation, sexual dysfunction, and pelvic pain. These problems can significantly affect the quality of life and can be treated with the help of a board-certified and experienced urogynecologist.
Urogynecology involves the diagnosis and treatment of the following conditions:
- • Urinary Incontinence
- • Incomplete Bladder Emptying
- • Pelvic Organ Prolapse
- • Overactive Bladder
- • Urinary Urgency
- • Urinary Frequency
- • Sexual Dysfunction
- • Vaginal Mesh Complications
- • Endometriosis
- • Pelvic/Vaginal Pain
- • Fecal Incontinence
- • Painful Bladder Syndrome
- • Recurrent Urinary Tract Infections
- • Atrophic Vagina
- • Vaginal Laxity
Stress Urinary Incontinence
Afraid to laugh, cough, or sneeze in public? You are not alone.
If you are living with stress urinary incontinence (SUI), whether it’s from childbirth, surgery, or age, we are excited to offer you an innovative new therapy.
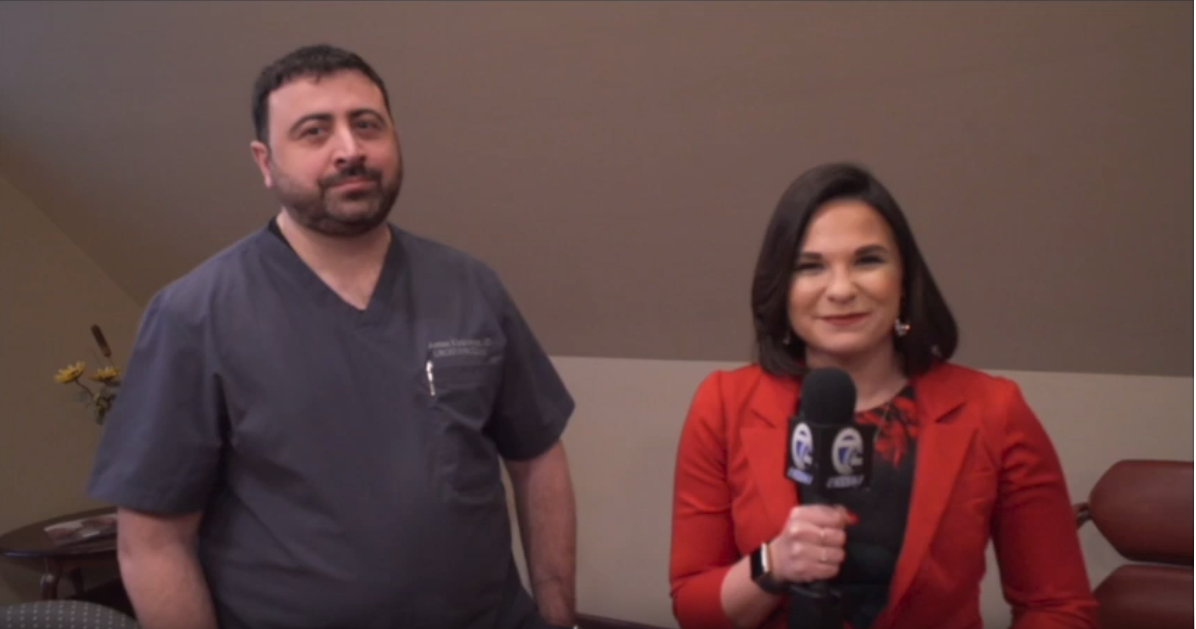
Dr. Armen Kirakosyan is the first in Western New York to offer this minimally invasive and effective treatment using FDA-approved Bulkamid® - a non-mesh, non-surgical, water-based hydrogel.
What is Stress Urinary Incontinence (SUI)?
SUI occurs when an individual experiences involuntary urine leakage due to a sudden pressure on the bladder. Mild cases occur with activities such as exercise, sneezing, laughing or coughing, while more severe cases occur when everyday activities such as standing up or walking cause leakage. The amount of leakage can vary from a few drops to enough to soak through clothes.
How Does Bulkamid Work?
The Bulkamid gel is injected into the soft tissue of the urethra using a syringe. The natural, safe hydrogel thickens the urethral tissue close to the opening of the bladder and creates a seal that helps prevent the loss of urine when the bladder is met with sudden pressure.
About the Procedure:
- • Performed in the doctor’s office
- • Takes 10-15 minutes
- • No downtime - most women resume normal activity the same day
- • Immediate relief of symptoms for the majority following the procedure
- • Effective treatment - long-term studies show 80% success rates lasting more than 5-7 years
Office Procedures:
Catheterization: Use of a very small sized catheter to drain urine from the bladder. This may be done to determine if you empty your bladder appropriately, or to collect urine specimens to send to the lab.
Cystoscopy: a procedure that involves placing a tiny camera through the urethra into the bladder to visualize the inner surface of the bladder.
Urodynamic Testing: a bladder function test involving the use of a tiny catheter in the bladder and one in the vagina or rectum. The bladder is filled with sterile water to assess the function of the bladder and urethra as well as the function of muscles and nerves. This test can help determine the reason for leakage of urine, urgency and/or the reason for the inability to empty the bladder well.
Conservative Treatment Options:
Dietary and lifestyle changes: A modifications in a diet to try to avoid products known to be bladder irritants. Water and drinks management is very important as well as physical activity and weight loss.
Bladder Training: Training your bladder to hold urine longer by doing pelvic floor exercises when you have an urge to urinate and allowing that urge to pass prior to urinating. The amount of time holding your urine increases incrementally over time.
Pelvic Floor Physical Therapy (PFPT): Meeting with a pelvic floor physical therapist to better understand the exercises involved in strengthening the pelvic floor muscles. PFPT treats many issues including vaginal prolapse, urinary incontinence, fecal incontinence, pelvic muscle weakness, and pelvic pain.
Pessary: A device that is placed in the vagina to support a vaginal prolapse and/or treat leakage of urine. A pessary fitting is done to determine which pessary type and size may be right for you. Sometimes you may need to try a few pessaries until you find the right pessary for you
Surgical Treatment Options:
Female pelvic reconstructive surgery: surgeries that restore the normal anatomy of female pelvic organs. A minimally invasive approach is usually utilized (laparoscopic or robotic surgery). This surgery may or may not involve hysterectomy. The use of synthetic or graft materials may be sometimes offered to patients as well to achieve the best results.
Types of Reconstructive Surgeries:
- • Sacrocolpopexy,
- • Uterosacral ligament suspension,
- • Sacrospinous ligament suspension,
- • Anterior, and Posterior Colporrhaphy, Perineorrhaphy.
Anti-Incontinence Surgeries:
Periurethral bulking injections: during cystoscopy, a tiny needle is used to inject a substance into the urethra to bulk up the urethra to reduce urinary incontinence that occurs with activity.
Bulkamid:This is a NEW procedure where gel is injected into the soft tissue of the urethra; it thickens the urethral tissue close to the opening of the bladder, creating a seal that helps prevent the loss of urine. Dr Kirakosyan is currently the only doctor in WNY to perform this procedure.
Sling: A surgical procedure in which a small, thin ribbon of mesh is placed through a vaginal incision under the urethra to reduce urinary incontinence that occurs with coughing, laughing or activity.
Burch procedure: the procedure was introduced in the 1950s. Still being used as effective anti-incontinence surgery and involves placing sutures on both sides of the urethra to create the necessary support and treat stress incontinence. It can be done via an open or minimally invasive approach.
Urgency treatments:
Sacral neuromodulation: A procedure that involves placing a small lead into the tailbone and a stimulating device in the area of where your hip pocket would be. This device works as a pacemaker to the bladder nerves to treat urge related urinary incontinence, frequent urination, incomplete bladder emptying, bladder retention, and fecal incontinence.
Percutaneous tibial nerve stimulation (PTNS): An office procedure involving the placement of a very small, acupuncture needle in the ankle and attaching the needle to a small device to stimulate the nerves that go to the bladder. This procedure gives off a signal to the bladder nerves to treat urge related urinary incontinence, urgency, and frequent urination. Each session lasts 30min. It is repeated weekly for 12 weeks, and then monthly as needed.
Bladder Botox injections: Injection of botox in the bladder wall during cystoscopy to relax the muscles of the bladder. This treatment temporarily treats urge related urinary incontinence and frequent urination. The effect lasts usually for 6-9 months. It can be periodically repeated to maintain efficacy.
Many treatments do not require surgery. However, when surgery is necessary, Dr. Kirakosyan offers a cutting-edge, minimally invasive approach.

 APPLY ONLINE TODAY!
APPLY ONLINE TODAY!